In this section you will find information on transfers from scene, inter-hospital transfers and repatriation transfers.
- Transfers from scene
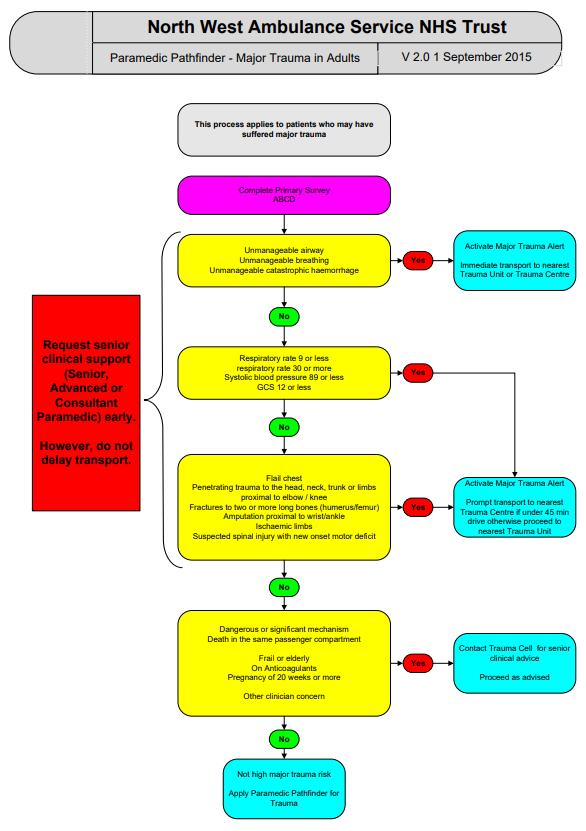
North West Ambulance Service have a numbers of pathways with the aim of transferring the patient to the ‘right place, first time’. For major trauma patients this is known as the NWAS Major Trauma Pathfinder (2015) and will direct patients to the Major Trauma Centre, should they require the services of a specialist centre.
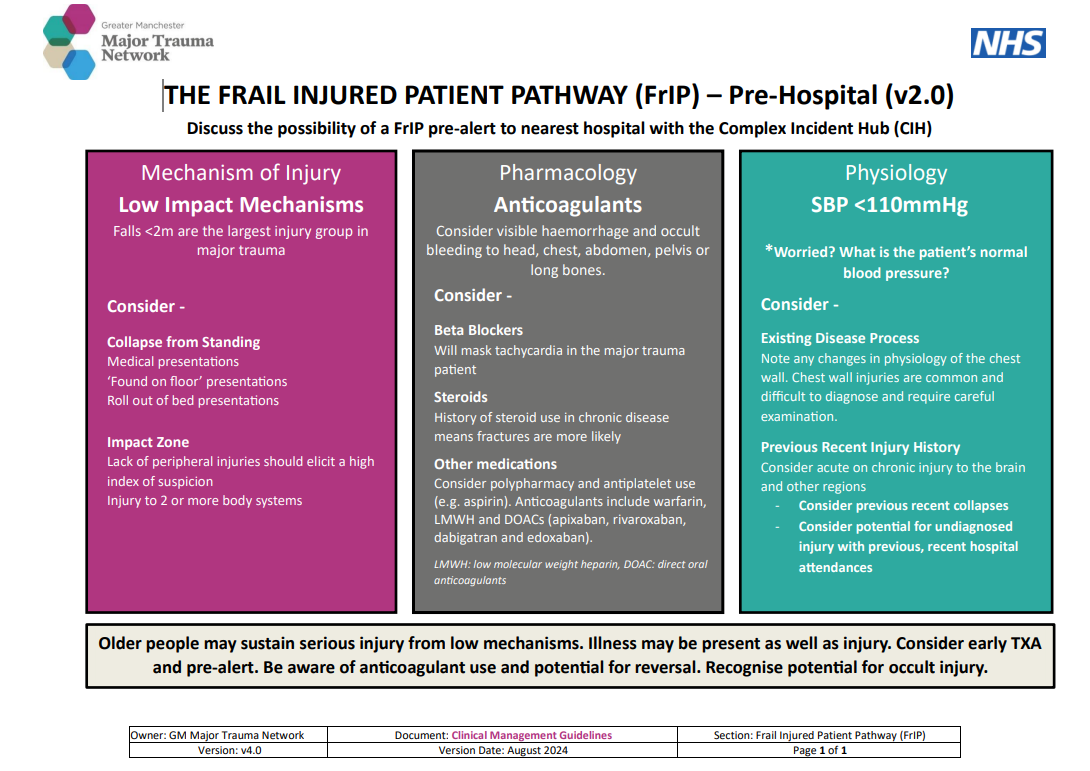
- Older patients in Greater Manchester
While the 2015 Pathfinder is utilised for all adult patients across Greater Manchester, it has been recognised that due to altered physiology and typically low mechanisms of injury, the over 65 age group are complex to identify as major trauma. This subgroup are the largest group of major trauma patients nationally; around 48% are falls <2m in people aged over 65 years. Many are ill as well as injured and sustain injuries following falls from standing height. This adds to the complexity of recognition and the Network has targeted project work around improving recognition in both the pre-hospital phase and ED reception. The Network have produced a secondary method of capture for this group known as the Frail Injured Patient Pathway or ‘FrIP’.
- The ‘FrIP’ Process
Patients that present as having potential major trauma injuries but do not fit the NWAS Major Trauma Pathfinder (known as ‘pathfinder negative’ patients) should be discussed with a senior paramedic on the Trauma Cell. Following discussion if the senior clinician agrees there are concerns, this may result in a pre-alert (via the ‘One Response’ screen) the nearest hospital of their imminent arrival. The purpose of the pre-alert is to inform the hospital site of an older patient with potentially serious injuries. How sites respond to this pre-alert is according to local hospital policy.
Early recognition, early senior review and timely, appropriate diagnostics have all been shown to improve outcome of this vulnerable group.
- Critically ill trauma patients in Greater Manchester
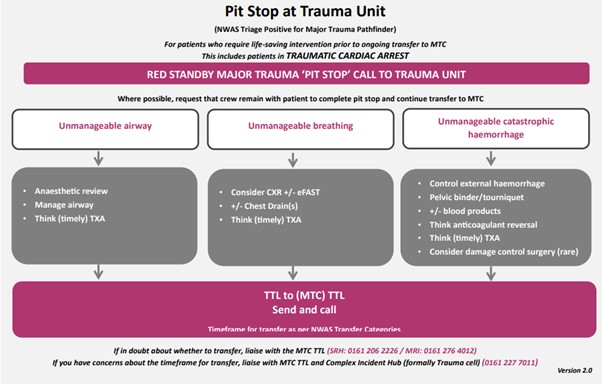
On occasion patients may be suffering from injuries that without rapid, expert intervention could result in serious disability or death. Examples include problems with
- unmanageable airway
- unmanageable breathing
- unmanageable, catastrophic haemorrhage
These patients require rapid identification and may require a ‘pit stop’ at the nearest Trauma Unit (TU) for intervention before onward travel to the MTC can be safely arranged. Patient’s in traumatic cardiac arrest fall into this category. The Pit Stop Pathway includes guidance on how to manage these patients
- Transfers from the Emergency Department
Patients identified as being ‘NWAS Major Trauma Pathfinder negative’ are conveyed to the nearest Emergency Department for assessment and if appropriate, diagnostics. Once an assessment has taken place and injuries are identified it may be appropriate to discuss patients with specialists based at other sites such as the MTC.
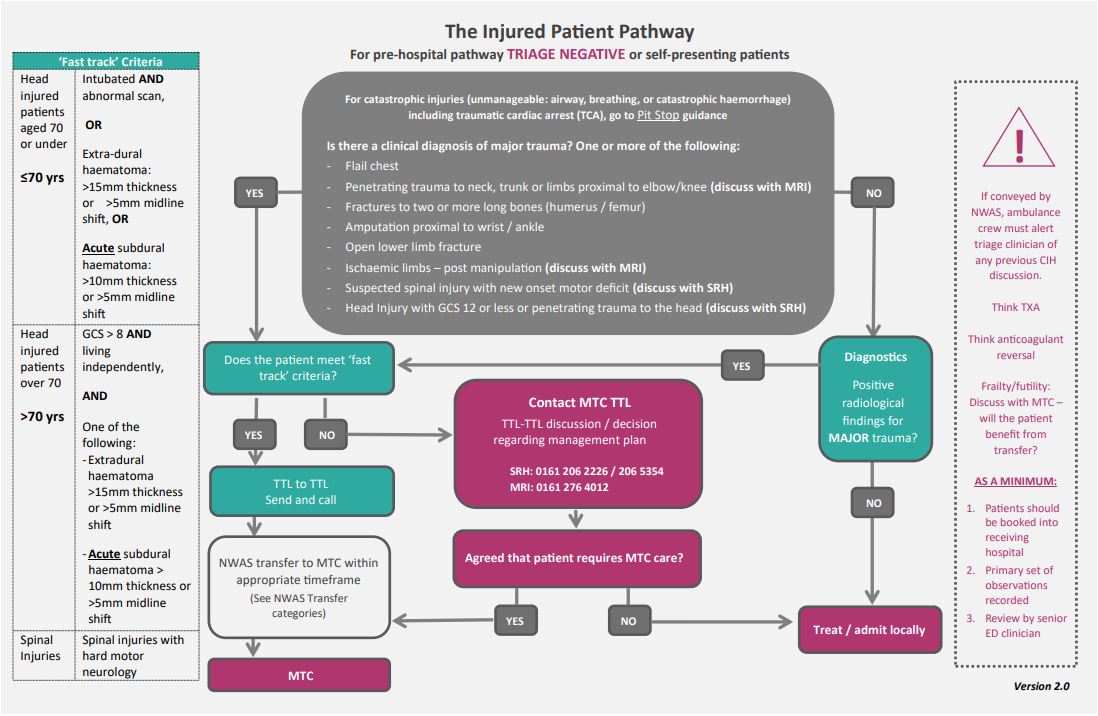
The Greater Manchester Injured Patient Pathway was launched in July 2019 . The pathway includes patient groups that should be automatically conveyed to the MTC and the process for discussion/onward transfer along with minimum standards of care.
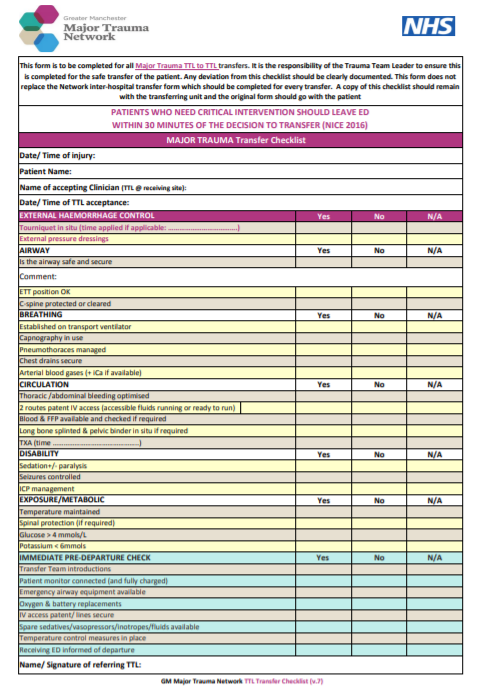
To promote safe transfer from one facility to another the Network has devised a TTL to TTL Transfer checklist that can be utilised by both the sending and receiving sites. A Network inter-hospital transfer form should also be completed as a record of the patient’s management during transfer
- Transfer from the MTC with completion of MTC care
To enable Major Trauma Centres (MTCs) to provide trauma care for the most severely injured patients on a continuous basis, it is essential to have a system in place to enable patients to return to a suitable local hospital as soon as the acute phase of their trauma care is completed. This enables them to continue their treatment closer to home and helps provide capacity for the MTC to continue to function as a hub within the network. The repatriation of major trauma patients to their local hospitals has the potential to be challenging for the patient, carers and organisations involved.
Unnecessary delays are unhelpful in a number of ways:
- They can prevent acutely ill patients being admitted into designated beds
- They can impede care packages for patients
- They can be inconvenient or distressing for both patient and relatives
- They can be a source of frustration in relationships between hospitals
This procedure aims to provide guidance to ensure a sustainable trauma service where delays are at the minimum; with robust escalation procedures should a delay occur. The Reverse Transfer Policy (updated September 2019) facilitate timely, safe and appropriate reverse transfer / repatriation of trauma patients within the GM Major Trauma Network by standardising the transfer of care processes from one organisation to another